Over your pregnancy? Baby is late? You’ve begun to ask “Can I ask to be induced?” When there’s no medical need for induction of labor, elective induction for convenience is not a decision to take lightly . Here’s what you need to know.
Your belly is so in the way. You can’t bend over to tie your shoes. Heck, you can’t bend over for anything! Picking up anything you drop is beyond awkward as you have to spread your legs and squat, all the while hoping you don’t topple over.
Sometimes you wonder if you should just be induced and get it all over with.
Nearing the end of your pregnancy, you’re likely exhausted and just want to get your body back. I’ve been there twice and can totally relate to it all. In fact, I narrowly escaped medical induction when my son was 13 days past his due date.
I totally understand what it’s like to be completely over the pregnancy.
Plus, how many more times can you answer the same questions like “when do we get to meet the baby?” If you’re getting these questions, be sure to read my post on all the other ways to irritate a woman whose pregnancy is overdue.
Your doctor has probably mentioned, at least once, that induction is an option. If she hasn’t, you’re probably thinking now would be a good time to meet the baby. And you may wonder “can I ask to be induced?“
But, requesting induction of labor isn’t a decision you should make so lightly.
Let’s discuss some of the common reasons and myths to help you determine whether or not you should be induced.

Can I Ask to Be Induced? Key Considerations Before Elective Induction
Whether or not you should begin to consider medical induction varies on a great many factors. I don’t believe that decision should be made without arming yourself with knowledge.
So, if you’re thinking of requesting induction, I want to help you understand a few things before you decide.
1. What’s Your Childbirth Goal?
Let’s FIRST determine what your ultimate goal is for your birth choice.
If you don’t really have an image of your perfect birth and are okay with medical interventions, up to and including C-Section, you may not need any of the following information. It’s totally okay if you’re cool with any outcome, but it won’t hurt you to know this either.
However, if your end game is to give birth naturally, it’s important to do some research before requesting induction. Be sure to become familiar with all these points before determining if you should be induced.
Cascade of Interventions
If your ultimate childbirth goal is a natural, drug-free birth, be aware that every medical intervention you accept, including elective induction, increases your chances for spiraling down the cascade of interventions.
The cycle is best outlined by Childbirth Connection in their article about the cascade of interventions:
Many maternity care interventions have unintended effects during labor and birth. Often these effects are new problems that are “solved” with further intervention, which may in turn create even more problems. This idea that using one intervention can lead to the need for more interventions is called a “cascade of intervention.”
The maternity practices that can lead to a cascade of intervention include:
- Using various medications to induce labor.
- Artificially breaking the membranes surrounding the baby and releasing amniotic fluid before or during labor.
- Using synthetic oxytocin medicine (“Pitocin”) to make labor move faster.
- Giving medications for pain relief.
- Laboring in bed versus being upright and moving about.
In many instances, these practices cause problems because they disrupt the normal physiology of pregnancy, labor and birth by:
- Interfering with hormones that move labor and birth along.
- Creating opportunities for infection.
- Having undesirable effects on your baby.
- Making it harder for you to push your baby out.
When these effects happen, women may feel that their bodies have failed them, not realizing that the things that went wrong could have actually been triggered by maternity practices themselves.
2. About Your Baby’s Due Date
First, please consider that a date you are given is based on a 40-week “average”. In pregnancy, a due date isn’t a guarantee, rather an estimation.
In 2013, the ACOG published the following in regard to defining term and post-term pregnancies:
“…recommended that the label “term” be replaced with the designations early term (37 0/7 weeks of gestation through 38 6/7 weeks of gestation), full term (39 0/7 weeks of gestation through 40 6/7 weeks of gestation), late term (41 0/7 weeks of gestation through 41 6/7 weeks of gestation), and postterm (42 0/7 weeks of gestation and beyond) to more accurately describe deliveries occurring at or beyond 37 0/7 weeks of gestation.”
It’s important to note that ACOG suggests a baby is overdue when it reaches 42 weeks or beyond. For this reason, I would not consider requesting induction before 42 weeks. It is generally known that first-time mothers often go into labor later than subsequent pregnancies, so it’s best to give your body (and baby) the time it needs to complete its job.
Additionally, it is no longer recommended to induce labor before 39 weeks, especially on an elective basis, unless medically necessary.
4 things to know if baby is late and 5 ways to cope
When Your Doctor Changes Baby’s Due Date
According to an Open Journal of Medical Imaging, in 2014, they state this about third trimester gestational age determination:
“[1]. Ultrasonic studies have proven useful in determination of gestational age (GA) in first and second trimester, but their accuracy in third trimester is not reliable because of biologic variations like racial differences in fetal biometric measurements and inter-population variations [2].”
Stick to your original EDD (expected due date) given from your LMP (last missed period) or the first trimester dating ultrasound (if you have one). If your doctor wishes to change your baby’s due date later in your pregnancy, especially after a third trimester ultrasound, respectfully decline. Of course, if your doctor wants to change the EDD to give you a few extra days, take it.
With my first baby, my doctor told us when he expected our baby would arrive, however, there was a bit of uncertainty over conception dates because of my irregular periods, so we pushed the due date out a few days later. As it would turn out, that baby arrived exactly on our chosen date on her own.
3. Baby’s Size or You’re Too Small
When I hear that a woman is being induced because her doctor is “worried the baby is too big” … frankly, I’m disappointed.
Don’t go getting defensive on me.
I’m disappointed in doctors for using these excuses to coerce a woman to be induced before either she or her baby are ready. The worst is when I hear “because they think I’m too small to deliver a baby naturally.”
I’m not all religious, but I’m pretty sure if that higher power made it so that we were to procreate, he’d also not be a jerk making it impossible for small women to deliver. So, let’s consider these two points:
CPD
Have you been led to believe you should be induced because you’re too small?
CPD (or Cephalopelvic Disproportion) is a rare disorder. According to American Pregnancy Association, CPD is rarely diagnosed prior to the onset of labor. “During labor, the baby’s head molds and the pelvis joints spread, creating more room for the baby to pass through the pelvis.”
Additionally, their site says “According to the American College of Nurse Midwives (ACNM), CPD occurs in 1 out of 250 pregnancies.” You can read more about CPD on the American Pregnancy Association’s Website.
Baby’s Size
I’ll be honest here. I don’t have any facts to back up whether or not third trimester ultrasound measurements are accurate enough to make any decisions on induction. I totally believe, however, that you need to refer to all the other points in this article.
Speaking from personal experience, my son was nearly 8 lbs at birth. I was 5′ 3″ and had only weighed about 120 lbs at the end of my third trimester. At 88 lbs when I got pregnant, I could have easily been targeted as someone who was either too small or whose baby was too big. Not only was he relatively big, he was 13 days late and I had absolutely no issues delivering him naturally.
Remember – proper laboring positions will help your pelvis expand the way it’s intended to make room for your baby. And, baby’s head is flexible so that it can mold to fit through the birth canal. Neither your pelvis nor your baby is a fixed object working against this process!
4. Complications
There may be medical complications in which your doctor suggests that you be induced.
A few reasons medical induction may be necessary include but are not limited to:
- hypertension
- preeclampsia
- abnormal bleeding
- or the baby being in danger of not receiving nutrients from the placenta
5. Is Baby in an Optimal Position?
Let’s get a little bit personal for a moment. If you haven’t taken the time to read my son’s story about being 13 days late, I highly recommend it.
The gist of the story is that I narrowly escaped labor induction by 1 day. My Bishop Score (discussed in the next point) was barely above the number indicating it was barely ready for labor.
Additionally, my son’s head was stuck on a bone in my pelvis. An induction was very likely not going to be effective, our labor could have been traumatic with a prolapsed cord if they broke my water, and I stood a higher chance of labor ending in a C-section.
I escaped all of this when I figured out my baby was not only not in the optimal position, he was also stuck on a bone preventing him from engaging and starting labor.
If the baby’s position is of concern, check out Spinning Babies to see if you can get your baby into position for birth before you decide to be induced!

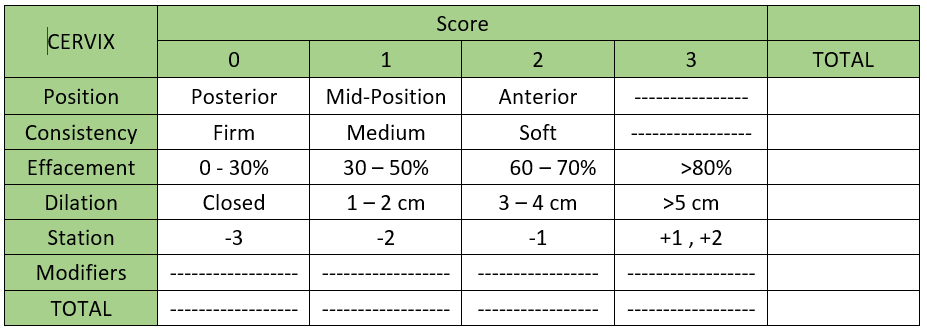
6. Is Your Cervix Ready? Check Your Bishop Score
Why is a Bishop Score Calculator Important Before Having An Induction?
If you’re thinking of requesting induction, you’re going to want to take into account whether or not your body is physically ready for labor, especially if you’re hoping to have a vaginal birth. ACOG describes the importance of your cervical readiness and how the Bishop Score helps to determine it:
“Health care providers use the Bishop score to rate the readiness of the cervix for labor. With this scoring system, a number ranging from 0–13 is given to rate the condition of the cervix. A Bishop score of less than 6 means that your cervix may not be ready for labor.”
Disappointingly, ACOG doesn’t discuss how they calculate your Bishop Score in this particular patient FAQ.
I believe it’s important to know your stats, so I’m sharing how to get your Bishop Score using a Bishop Score Calculator. You can read more about the Bishop Score from Family Practice Notebook and then sign up for my emails to get your own Printable Bishop Score Calculator for FREE.
7. Labor Induction Risks
Refer back to #1 where I discuss the cascade of interventions. Additionally, Mayo Clinic Lists the following risks of labor induction:
- The need for a C-section. Labor induction is more likely to result in the need for a C-section — particularly if you’ve never given birth before and your cervix hasn’t already begun to thin, soften and dilate (unfavorable cervix).
- Premature birth. Inducing labor too early might result in a premature birth. This poses risks for the baby, such as difficulty breathing.
- Low heart rate. The medication used to induce labor — oxytocin or a prostaglandin — might provoke too many contractions, which can diminish your baby’s oxygen supply and lower your baby’s heart rate.
- Infection. Labor induction increases the risk of infection for both mother and baby.
- Umbilical cord problems. Labor induction increases the risk of the umbilical cord slipping into the vagina before delivery (umbilical cord prolapse), which might compress the cord and decrease the baby’s oxygen supply.
- Uterine rupture. Uterine rupture is a rare but serious complication in which the uterus tears open along the scar line from a prior C-section or major uterine surgery. An emergency C-section is needed to prevent life-threatening complications.
- Bleeding after delivery. Labor induction increases the risk that your uterine muscles won’t properly contract after you give birth (uterine atony), which can lead to serious bleeding after delivery.
For me, personally, increasing the chances of a C-section was a huge deterrent in all the decisions I made about both my labors. Still, unless medically necessary, those possibilities don’t seem to be worth the risk of requesting induction unless it’s necessary.
Is it Okay to Have an Elective Induction?
The most important first step in deciding whether or not to consider elective induction is to know your ultimate childbirth goal. If natural birth is what you’re preparing for, remember that induction is the first step in the cascade of interventions so this decision shouldn’t be made lightly.
Knowing what is and isn’t a medical necessity prepares you for making the right decisions.
If there appears to be a medical necessity that requires you to be induced, knowing your Bishop Score will help you determine whether or not your body is likely to take to a medical induction, should you decide you want to go on with requesting induction.
FAQs about Elective Induction
Can I be induced early by request?
Barring medical reasons for induction, there is no benefit for requesting to be induced early. Remember that your baby is still growing and developing and that you should give him or her the time needed to be ready for birth.
Will insurance pay for elective induction?
Some insurance companies have adopted policies to exclude elective induction from reimbursement eligibility before 39 weeks if not medically necessary. We recommend to check with your insurance provider before making any decisions about the medical management of pregnancy and induction of labor.
Can I Choose How to Be Induced?
To some extent. Your provider will perform an assessment of your cervix and calculate a bishop score then provide the recommended induction option. He/she may provide options for you to consider based on your bishop score. But, you’re also allowed to decline or postpone induction if you’re not high-risk or in immediate danger.
Is it better to be induced or go naturally?
This choice will need to be made through a combination of understanding your childbirth goals and you personal circumstances. Arm yourself with the research and knowledge so that you can determine the best labor plan with a trusted medical provider.
How long does elective induction take?
This depends on whether or not you’re full-term, first or subsequent babies, and your body/cervix readiness. While inductions usually don’t take very long, it is possible for it to take several days, depending on your personal circumstances.
Is being induced harder labor?
This can depend on the type of induction you’re receiving. It’s said that contractions from medical induction are more intense and can last longer.
Can you eat during induction?
We recommend eating during labor while you’re at home, but if you’ve been medically induced and are at the hospital, you most likely will be restricted from eating.
This post, Elective Induction, originally appeared on SAHM, plus… August 2017 and has been updated.

10 comments
Great information here Ivy!!! I always encourage people to NOT get induced, even if they are past their due date! Obviously, listen to your doctor IF there is a real medical need to be induced, but otherwise, don’t force it. Let baby come when he/she’s ready!
Thanks so much for stopping by and sharing!! It’s true baby will come when baby is ready.
I think the common misconception is that doctor knows best. While that can be true in certain situations, I’m testament to that not always being the case. My doctors never informed me that my son’s head was lodged on a bone preventing me from going into labor for so long. An induction would have complicated our situation greatly. I think there’s a fine line between listening to your gut vs. listening to a doctor IMO.
Very useful post Ivy. Even women who have wonderful, healthy and beautiful pregnancies are likely to be tired of being pregnant within a few weeks of their due dates. Feeling heavy, bloated, and tired, these mamas are ready to give birth. Being pregnant requires one to let go of the idea that pregnancy, labor, birth, or parenting will ever be convenient. I remember being 40 weeks pregnant and wishing it was over. I even tried to induce myself, which didn’t work very well. In the end, I’ve come to realize that my time is better spent getting rest, getting pampered, and using it to grow patience useful for parenthood.
Best wishes!
I just wanted to say that I loved this! With my second, I was able to have my VBAC and they actually told me that I could not be induced because of it. I ended up going a little over 41 weeks before he was born, and was able to “miss” my scheduled repeat C-section date!
Thanks for sharing. very useful for me
Thanks for the share, this information is extremely useful!
Alison, Of course! Thanks for reading 🙂
Thank you so much Ivy, this was so helpful especially knowing how stressful and difficult pregnancy can be.
I just wanted to comment on the fact that I adored this! I was fortunate to have a vaginal birth after caesarean section with my second child, and as a result, I was advised that I could not be forced into labour. I had planned to have a repeat caesarean section, but since I went a little over 41 weeks before giving birth to him, I was able to “miss” the date!
Thank you for sharing a very meaningful article, I think it will be very helpful for me and everyone.
Comments are closed.